FSA Administration For Employers: Compliance & Guidelines
As a pre-tax account that allows employees to cover qualified healthcare expenses, a Flexible Spending Account (FSA) can be a good way to boost your employee benefit offerings with minimal costs to you. So it’s no surprise that 63% of companies today offer FSAs. If you’re thinking about offering an FSA to your employees, you may be wondering what FSA administration rules you need to follow to stay compliant. Let’s find out.
In this article, we’ll discuss the guidelines employers are required to follow for FSAs, including rules for setting up an FSA, contribution requirements, claims substantiation, Form 5500 filing, and more. After reading this, you’ll be prepared to properly administer a healthcare FSA and will better understand whether it may make sense to outsource administration to an FSA TPA to ensure compliance with the complex legal requirements.
It’s important to note that you can also offer a dependent care FSA that allows employees to set aside up to $5,000 pre-tax to cover qualified daycare expenses. However, for the purposes of this article, we’ll focus on the administration of a health flexible spending account.
How do I set up an FSA?
The first step in offering an FSA is to identify a bank, credit union, insurance company, payroll company, or third-party administrator to manage your accounts. You’ll then want to work with them to design your FSA plan. That means deciding things like how much you as an employer will contribute, if at all, whether you want to offer a debit card, and if you want to allow a grace period or carry over for unused funds at the end of the year.
Next, you’ll need to provide bank account information for claims reimbursements to the financial institution who will manage your FSA accounts. You’ll then supply an enrollment list and collect FSA election forms from participating employees.
In the election forms, employees will need to select their annual contribution amount. This is the only time during the year they can elect a contribution amount unless they have a specific qualifying event in their life, which we’ll talk about later.
How are FSAs funded?
FSAs are usually funded through voluntary salary reduction agreements with you as the employer. That means the employee contributes to their FSA by electing an amount to be voluntarily withheld from their pay. For 2023, salary reduction contributions to a health FSA can’t be more than the IRS limit of $3,050. Depending on how you set up your plan, you may also be able to contribute to your employees’ FSAs. FSA funds are immediately available to the employee for use from the first day of the plan year.
Regardless of who makes the contributions, they’re excluded from the employee’s gross income so your workers save on income taxes. This is a big bonus because both you and your employee save on payroll taxes.
In addition to tax-free contributions, employees are reimbursed tax-free for their claims as long as they use the money to pay for qualified medical expenses.
One feature that makes an FSA unique from other tax-advantaged plans is that FSA funds that aren’t used at the end of the year are sent back to the employer unless the plan has a grace period or carryover feature. You can use these plan gains for certain activities like defraying FSA administration costs.
What’s involved in administering an FSA?
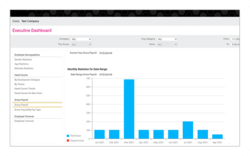
The reason most employers choose to outsource their FSA administration to a third party administrator (TPA) is because there’s a lot of responsibility that comes with administering these plans. Some of the activities that need to take place during the plan year include:
- Educate employees through marketing and enrollment materials to encourage participation
- Manage enrollment and set up employee accounts
- Provide ongoing funding management
- Issue debit cards
- Process claims
- Certify submitted expenses
- Handle reimbursements
- Make forfeiture determinations
By outsourcing some or all of these tasks to an FSA administrator, you’ll alleviate the burden on your own staff and provide a simplified plan experience for you and your employees.
What do I need to do to be compliant with FSA rules?
Not only are there a lot of steps involved with administering an FSA, but you’ll also have to follow the guidelines established in Section 125 of the Internal Revenue Code as well as other FSA rules to avoid problems.
Here are 10 things you can do to avoid some of the most common compliance issues employers face when it comes to FSA administration.
1. Creating Plan Documents
Since an FSA is a health plan governed by ERISA, you’ll need to comply with the law’s provisions, one of which is that you provide a Summary Plan Description (SPD) about the plan to participants. You’ll also need to create a written plan document that outlines conditions for eligibility, benefits and rules.
2. Ensuring Proper Claim Substantiation
When employees use FSA funds, they’ll need to show that what they used the pre-tax dollars for was an eligible expense, such as deductibles and copayments, doctor and dentist visits, medications, and medical equipment like bandages and blood sugar test kits.
You’ll need to set up procedures for substantiating these claimed medical expenses. If you use an FSA TPA who offers a benefits debit card, some systems will automatically approve funds while, for others, employees may need to provide documentation or receipts.
3. Dealing with Unused/Forfeited FSA Funds
FSAs are “use it or lose it” plans. That means that, at the end of the year, the employee forfeits any unused funds in their accounts. However, there are some exceptions. You can design your plan to allow a grace period of up to 2.5 months or a carryover amount up to $610 for 2023.
If employees still have unused funds, you can use the amounts for certain activities, including paying reasonable FSA administration fees or reducing payroll deductions for all employees the following plan year by the amount you’re contributing from forfeited funds.
4. Adhering to the Contribution Cap
Each year, there may be changes to the IRS limit of pre-tax contributions your employees can put into a healthcare FSA, either on their own or with your help. As we mentioned earlier, for 2023, the cap for FSAs is $3,050. You’ll want to make sure plan documents reflect the contribution limits each year.
5. Limiting Election Changes
With an FSA, employees can only set their contribution limit once, at the start of the plan year, unless they have a qualifying event mid-year. Examples of qualifying events include:
- Change in marital status
- Change in number of dependents
- Change in employment status
6. Performing Non-discrimination Testing
One of the rules for FSAs is that they be offered on a non-discriminatory basis. To show your compliance with this requirement, each year, you or your FSA administrator will need to complete non-discrimination testing to prove that the plan doesn’t favor highly-compensated employees, officers or owners. This involves conducting tests regarding eligibility, contributions and benefits, and key employee concentration.7. Ensuring ACA Compliance
Your plan must qualify as an excepted benefit, or coverage that isn’t included in a traditional health insurance plan, to avoid certain requirements under the Affordable Care Act. An FSA is considered to provide only excepted benefits if you also make available a group health plan and any contributions you make as the employer don’t exceed the greater of the employee’s salary reduction or $500.
8. Filing Form 5500
As part of your FSA administration responsibilities, you’re required to file Form 5500 with the IRS each year if your FSA has 100 or more participants to report information about the plan. If you offer more than one health and welfare plan and have a wrap plan document, you can just file one Form 5500 for all the plans rather than separate forms.
Form 5500 is due the last day of the seventh month after the plan year ends. For example, the due date would be July 31 for a calendar-year plan or the next business day if July 31 is on a weekend. The form must be filed electronically using EFAST2.
9. Providing COBRA Coverage
Since an FSA is generally considered an ERISA-covered plan, you’ll need to offer COBRA continuation coverage for qualified beneficiaries. You’ll have to offer COBRA regardless of whether the account is over- or underspent.
10. Meeting HIPAA Requirements
A healthcare FSA (other than a self-administered plan with fewer than 50 participants) is considered a group health plan and is subject to HIPAA privacy standards around protected health information (PHI).
If you’re handling your own administration instead of using an FSA administrator, you’ll need to distribute a Notice of Privacy Practices, limit access to PHI, and implement safeguards to protect it when reviewing claims or receipts for medical expenses.
What are possible penalties for non-compliance?
The fines for non-compliance with FSA rules and regulations can quickly add up. Here are some examples:
- If you don’t file a Form 5500, you may have to pay a Department of Labor fine of up to $2,400 a day plus IRS penalties of $250 per day.
- If you don’t meet the COBRA notice requirements, you could be fined $110 a day per qualified beneficiary by the DOL plus the IRS could impose an excise tax.
- You can even face a penalty of up to $60,973 for HIPAA violations you didn’t know about.
There can be other financial consequences to your business as well. If your plan fails to meet the substantiation requirements and pays ineligible expenses from a FSA, it can be deemed an “operational failure” and the entire plan could be disqualified. That could make you responsible for an employment tax withholding liability and penalties for all employee pre-tax and elective employer contributions.
How to Best Stay FSA Compliant
As you can see, there are many technical steps involved in correctly administering a health Flexible Spending Account. That’s why most companies choose to outsource their FSA administration duties to a TPA to ensure compliance. If you choose to go this route, there are lots of providers out there. To help you make a decision, read our next article on the top factors to consider when choosing a TPA.
Editor’s Note: This post was originally published in December 2020 and was updated in January of 2023 for comprehensiveness.
in
 Benefits
,
FSA
,
Pre-Tax Benefits
Benefits
,
FSA
,
Pre-Tax Benefits